Moderate Brain Injury: 3 Critical Types
What You Need to Know About Brain Injuries
Moderate brain injury sits in a critical middle ground on the traumatic brain injury (TBI) spectrum—more serious than a concussion but not as immediately life-threatening as a severe TBI. Here’s what defines it:
- Loss of consciousness lasting between 15 minutes and 6 hours
- Post-traumatic amnesia (confusion and memory gaps) lasting up to 24 hours
- Glasgow Coma Scale score between 9 and 13
- Common symptoms include persistent headaches, dizziness, memory problems, difficulty concentrating, and irritability
- Recovery timeline typically ranges from 6 to 9 months, though some effects may be permanent
- Hospitalization is usually required for observation and treatment
The brain is the control center for everything you do—every thought, movement, and emotion. When a violent blow or jolt injures your head, it can disrupt how your brain functions. Not all head injuries are the same. A traumatic brain injury (TBI) occurs when external force damages brain tissue, and these injuries exist on a spectrum from mild to severe. Understanding where a moderate brain injury falls on this spectrum is crucial for getting the right medical care and recognizing the long-term challenges ahead.
Falls are the leading cause of TBI-related hospitalizations, especially for older adults. Motor vehicle crashes, assaults, and sports injuries also account for thousands of moderate to severe brain injuries each year. The lifetime economic cost of TBI in the United States was estimated at $76.5 billion in 2010 dollars, and that number continues to rise.
As Thomas W. Carey, I’ve spent decades representing individuals and families affected by traumatic brain injuries caused by negligence. Throughout my career handling moderate brain injury cases, I’ve seen how these injuries can transform lives—and how critical it is to understand what you’re facing.
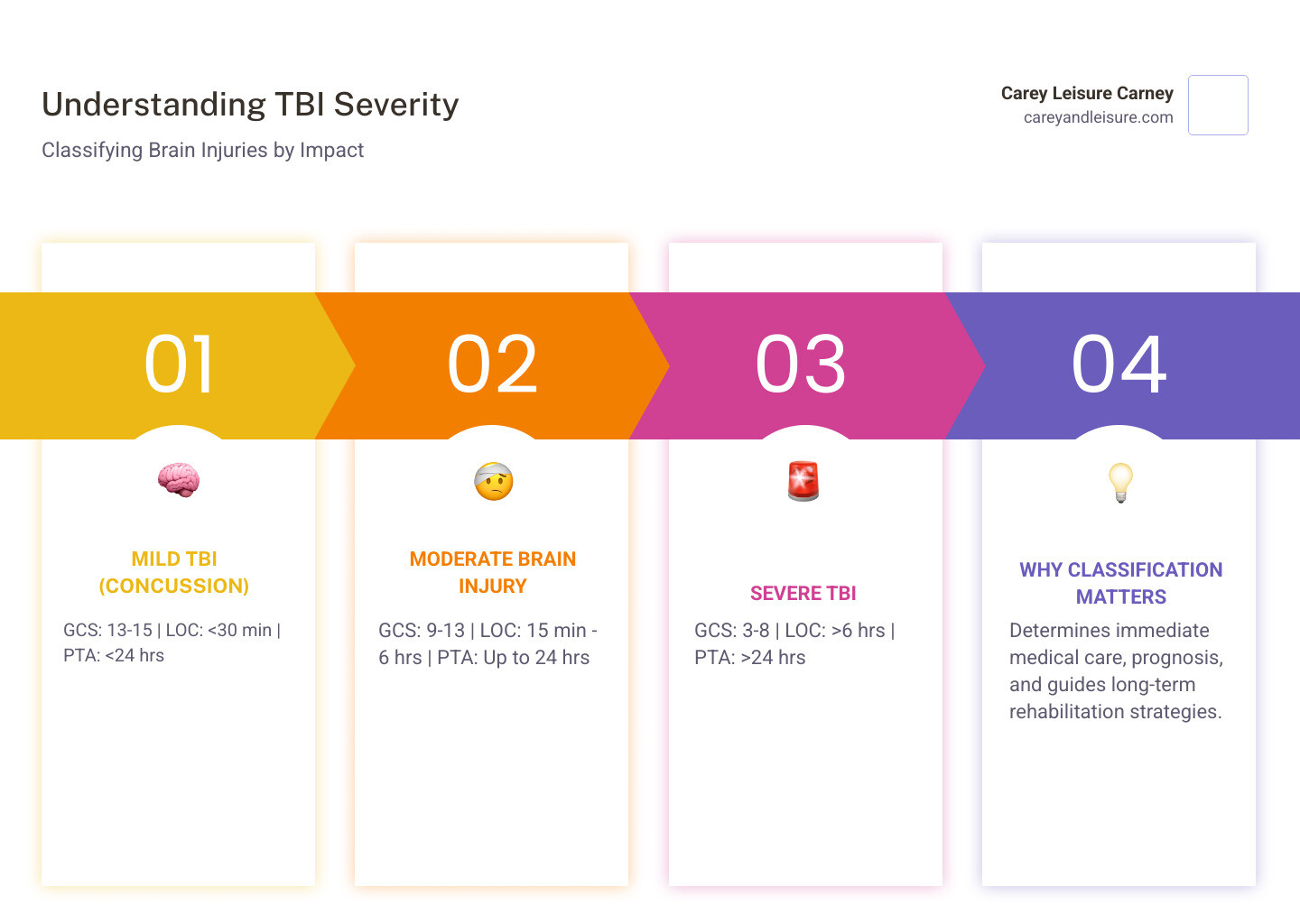
Understanding TBI Severity: Mild, Moderate, and Severe
To truly grasp the complexities of a moderate brain injury, we first need to understand how traumatic brain injuries are classified. The severity of a TBI is primarily assessed using several key indicators that help medical professionals gauge the immediate impact on brain function. These include the Glasgow Coma Scale (GCS) score, the duration of loss of consciousness (LOC), and the length of post-traumatic amnesia (PTA). This classification helps guide immediate treatment and provides an initial prognosis for recovery.
| Severity Level | Glasgow Coma Scale (GCS) | Loss of Consciousness (LOC) | Post-Traumatic Amnesia (PTA) |
|---|---|---|---|
| Mild TBI | 13-15 | Less than 30 minutes | Less than 24 hours |
| Moderate TBI | 9-12 | 15 minutes to 6 hours | Up to 24 hours |
| Severe TBI | 3-8 | More than 6 hours | More than 24 hours |
Mild TBI (Concussion)
A mild TBI, often referred to as a concussion, is the most common type of brain injury. While it might seem “mild” in name, its effects can still be significant and should never be underestimated. A concussion occurs when a bump, blow, or jolt to the head causes the brain to move rapidly inside the skull, leading to temporary disruption of brain function.
Symptoms of a mild TBI can include headache, confusion, dizziness, nausea, memory problems, and sensitivity to light or sound. While these symptoms are often temporary, typically clearing up within a few weeks or months, proper “brain rest” is crucial for healing. Ignoring a concussion and returning to strenuous activities too soon can lead to a more prolonged recovery or even a dangerous condition known as Second Impact Syndrome, where a second injury before the first has healed can cause catastrophic damage. If you’re experiencing lingering symptoms, it’s important to understand more on post-injury symptoms.
Defining a Moderate Brain Injury
This is where our focus truly lies. A moderate brain injury is a more serious event than a concussion, positioned squarely between mild and severe TBIs. It is typically defined by:
- Loss of consciousness: The individual may be unconscious for a period ranging from 15 minutes up to 6 hours.
- Post-traumatic amnesia (PTA): This refers to a state of confusion and disorientation after the injury where the person may not remember events that occurred for up to 24 hours. They might seem aware but are confused and can’t form new memories during this time.
- Glasgow Coma Scale (GCS) score: A GCS score between 9 and 12 indicates a moderate brain injury. This scale assesses eye-opening, verbal response, and motor response.
Following a moderate brain injury, hospitalization is almost always required. This allows medical professionals to closely observe the patient for any worsening symptoms, such as swelling or bleeding in the brain, and to stabilize their condition. While many individuals with a moderate brain injury see significant improvement, there is a higher potential for lasting deficits compared to mild TBIs. These deficits can impact physical, cognitive, and emotional functions, necessitating comprehensive rehabilitation and support. For a more comprehensive overview of symptoms across the TBI spectrum, you can refer to detailed symptoms of TBI.
Severe TBI
At the most critical end of the spectrum is a severe TBI. This diagnosis signifies extensive brain damage and is characterized by a loss of consciousness lasting more than 6 hours, or post-traumatic amnesia extending beyond 24 hours. Patients with severe TBI often fall into a coma or other states of altered consciousness, such as a vegetative state or minimally conscious state.
Severe TBIs are life-threatening and almost invariably lead to significant long-term impairment. These injuries require intensive medical intervention, often including surgery, and extensive, long-term rehabilitation. The prognosis for a full recovery is often guarded, and individuals may face lifelong challenges affecting every aspect of their lives.
Causes and Immediate Symptoms of a Moderate Brain Injury
Understanding how a moderate brain injury occurs and what signs to look for immediately afterward is critical for prompt medical intervention and potentially better outcomes. These injuries often result from powerful external forces impacting the head, leading to significant disruption of brain tissue and function.
Common Causes of Traumatic Brain Injuries
Traumatic brain injuries, including those of moderate severity, can stem from a variety of incidents, often involving sudden and forceful impacts. We frequently see these types of injuries in cases where negligence plays a role.
- Falls: These are the most common cause of TBIs across all age groups, especially among young children and older adults (age 75 and older). A fall from a ladder, down stairs, or even a simple slip and fall can generate enough force to cause a moderate brain injury.
- Vehicle-Related Collisions: Car accidents are a leading cause of moderate to severe TBIs. The sudden deceleration and violent impacts in these incidents can cause the brain to violently strike the inside of the skull, leading to bruising, swelling, and tearing of brain tissue. Whether it’s a head-on collision or a rear-end impact, the forces involved can be devastating. For more specific information, please see our page on Car Accidents and Traumatic Brain Injuries.
- Assaults and Violence: Acts of violence, such as physical assaults, can result in direct blows to the head that cause significant brain trauma.
- Sports-Related Injuries: While concussions are more commonly associated with sports, high-impact activities like football, soccer, or even cycling can lead to moderate brain injury if the impact is severe enough.
- Workplace Accidents: Certain occupations, particularly those involving heavy machinery, heights, or dangerous environments, carry a risk of head trauma that can result in moderate brain injuries. Examples include construction site accidents or falls from liftd platforms.
Recognizing the Immediate Signs of a Moderate Brain Injury
The immediate signs and symptoms of a moderate brain injury are typically more pronounced and alarming than those of a mild concussion. It’s crucial for anyone witnessing an incident or caring for someone who has sustained a head injury to be aware of these indicators and seek emergency medical care without delay.
According to the Centers for Disease Control and Prevention (CDC) and Mayo Clinic, immediate signs that suggest a moderate to severe TBI include:
- Persistent headache: A headache that worsens or doesn’t go away.
- Repeated vomiting or nausea: More than just a single instance of sickness.
- Seizures or convulsions: Uncontrolled shaking or muscle spasms.
- Dilation of one or both pupils: Unequal pupil size can indicate pressure on the brain.
- Inability to awaken from sleep: The person is difficult to rouse or remains unconscious.
- Clear fluids draining from the nose or ears: This could indicate a cerebrospinal fluid leak, a serious complication.
- Profound confusion, agitation, or combativeness: The individual may be deeply disoriented, restless, or aggressive.
- Slurred speech: Difficulty speaking clearly or coherently.
- Weakness or numbness in fingers and toes: This can indicate nerve damage or pressure on the spinal cord.
- Loss of coordination: Difficulty with balance or performing motor tasks.
- Coma or other disorders of consciousness: Prolonged unconsciousness beyond a brief period.
If you observe any of these symptoms after a head injury in Clearwater, Largo, New Port Richey, Spring Hill, St Petersburg, Trinity, or Wesley Chapel, Florida, it is imperative to get immediate medical attention. Time is of the essence in preventing further brain damage and improving long-term outcomes.
The Long-Term Impact and Road to Recovery
A moderate brain injury is not just a single, isolated event; it marks the beginning of a challenging and often lengthy process of healing and adaptation. The brain is incredibly complex, and even a “moderate” injury can lead to a wide array of lasting changes that affect an individual’s physical, cognitive, and emotional well-being. We understand that this journey can be overwhelming, not just for the survivor but for their entire family.

Potential Long-Term Physical, Cognitive, and Emotional Effects
The residual symptoms following a moderate brain injury are diverse and can significantly impact daily life. While some symptoms may gradually improve, others can become chronic or even permanent, fundamentally altering how a person functions.
Physical Effects:
- Tiredness and Fatigue: Persistent exhaustion that doesn’t improve with rest, making it difficult to maintain energy levels for daily tasks.
- Headaches: Chronic or recurring headaches, which can range from mild to severe.
- Dizziness and Vertigo: Feelings of lightheadedness, unsteadiness, or a sensation of spinning.
- Weakness or Numbness: Reduced strength or sensation in limbs, potentially affecting mobility and fine motor skills.
- Sensory Problems: Changes in vision (blurred, double vision, light sensitivity), hearing (loss, tinnitus, sound sensitivity), smell, or taste.
- Loss of Coordination: Difficulties with balance, gait, and performing coordinated movements.
- Seizures: The development of post-traumatic epilepsy, which can occur years after the initial injury.
- Sleep Disorders: Insomnia, excessive sleepiness, or disrupted sleep patterns.
- Chronic Pain: Persistent pain in various parts of the body.
Cognitive Challenges:
- Difficulties with Thinking and Information Processing: Slower processing speed, difficulty understanding complex information.
- Attention and Concentration Problems: Inability to focus, easily distracted, trouble sustaining attention.
- Memory Problems: Short-term memory loss, difficulty learning new information, or retrieving past memories.
- Planning and Organizing: Impaired executive functions, making it hard to plan tasks, manage time, or prioritize.
- Word-Finding Problems: Difficulty recalling specific words during conversation.
- Confusion: Persistent disorientation or mental fog.
- Impaired Judgment: Difficulty making sound decisions or understanding consequences.
Emotional and Behavioral Changes:
- Irritability and Anger: Increased frustration tolerance, sudden outbursts, or aggressive behaviors.
- Anxiety and Depression: Heightened feelings of worry, nervousness, sadness, or hopelessness.
- Emotional Lability: Rapid and unpredictable mood swings.
- Personality Changes: Alterations in typical personality traits, such as becoming more impulsive, withdrawn, or dependent.
- Lack of Motivation: Apathy or difficulty initiating activities.
- Social Difficulties: Trouble understanding social cues, inappropriate behaviors, or withdrawal from social interactions.
These long-term effects can combine to create significant challenges. For example, a person who was once an optimist might become depressed, or someone previously tactful might blurt out embarrassing comments. These are not character flaws but direct consequences of the brain injury.
Diagnosis and Rehabilitation
The journey to recovery from a moderate brain injury begins with prompt and accurate diagnosis. In the emergency room, doctors will perform a neurological exam to assess motor and sensory skills, reflexes, mental status, and behavior. The Glasgow Coma Scale (GCS) is a critical tool used to rate the severity of the injury. Imaging tests such as a CT scan or MRI are often ordered to look for signs of bleeding, bruising, swelling, or skull fractures in the brain.
Once the initial medical crisis is managed, the focus shifts to rehabilitation. This is a comprehensive process aimed at helping individuals regain as much function as possible. A multidisciplinary rehabilitation team typically includes:
- Physical Therapists: To improve strength, balance, coordination, and mobility.
- Occupational Therapists: To help relearn daily living skills, such as dressing, eating, and managing household tasks.
- Speech-Language Pathologists: To address communication problems, including speech, language comprehension, and swallowing difficulties.
- Neuropsychologists: To assess cognitive functions (memory, attention, problem-solving) and provide strategies for coping with cognitive deficits, as well as address emotional and behavioral issues.
- Rehabilitation Nurses: To manage medical needs and educate patients and families.
- Social Workers/Case Managers: To coordinate care, connect families with resources, and assist with discharge planning.
Rehabilitation can occur in various settings, including inpatient rehabilitation facilities, outpatient clinics, or even at home, depending on the individual’s needs. The goal is always to maximize independence and improve quality of life. For more information on brain injury rehabilitation programs and services, the CDC offers valuable resources.
The Recovery Process and Timeline
The recovery process from a moderate brain injury is highly individual and can be unpredictable. While the majority of people with a moderate brain injury experience gradual improvement in their residual symptoms, this can sometimes take 6 to 9 months. During this period, the brain is actively healing, and therapies are designed to retrain neural pathways and develop compensatory strategies.
However, it’s important to understand that for many, a moderate brain injury can lead to long-term or even lifelong health problems. The CDC notes that moderate to severe TBIs may lead to health problems that affect all aspects of a person’s life, similar to the effects of a chronic disease. This doesn’t mean recovery stops after 9 months; rather, it often transitions into managing a chronic condition.
Challenges in returning to work or school are common, as cognitive deficits like attention, memory, and organization can make previous roles difficult to resume. Individuals may feel they are not functioning at their peak, leading to frustration and reduced self-esteem.
Throughout this journey, a strong support system is invaluable. This includes family, friends, and support groups where individuals can share experiences and coping strategies. We also emphasize the importance of understanding your legal options. If your moderate brain injury was caused by someone else’s negligence, you may have rights to compensation for medical expenses, lost wages, and pain and suffering. Learning about understanding your legal options can provide crucial support during this challenging time.
Navigating Life After Injury: Challenges and Prevention
Life after a moderate brain injury presents unique challenges not only for the individual but also for their entire support system. At the same time, understanding prevention strategies is key to reducing the incidence of these life-altering events.
Challenges for Survivors and Their Families
The ripple effects of a moderate brain injury extend far beyond the injured individual. Families often find themselves navigating a complex landscape of medical appointments, rehabilitation sessions, and emotional adjustments.
- Daily Life Adjustments: Survivors may struggle with basic daily activities that were once second nature. Simple tasks like managing finances, cooking, or even personal hygiene can become difficult, requiring significant support and adaptation.
- Emotional Toll on Caregivers: Family members, particularly primary caregivers, often experience immense emotional strain. Watching a loved one struggle with cognitive, emotional, or behavioral changes can be heartbreaking and lead to feelings of stress, anxiety, depression, and burnout. The person they knew before the injury might seem different, which can be a profound loss.
- Financial Strain: The economic burden of a moderate brain injury can be devastating. Medical bills for emergency care, hospitalization, rehabilitation, and ongoing therapies can quickly accumulate. Furthermore, lost wages due to the inability to work—either for the survivor or a family member who becomes a caregiver—can lead to significant financial distress. The lifetime economic cost of TBI, including direct and indirect medical costs, was estimated at approximately $76.5 billion (in 2010 dollars), highlighting the massive financial impact.
- Navigating the Healthcare System: The healthcare system can be difficult to steer, with multiple specialists, insurance complexities, and varying levels of care. Families often need to become advocates for their loved ones, ensuring they receive appropriate and consistent treatment.
Prevention Strategies to Reduce Risk
While we can’t eliminate all risks, many moderate brain injuries are preventable. By adopting safety practices, we can significantly reduce the likelihood of these devastating events. This is especially true in our Florida communities like Clearwater, Largo, New Port Richey, Spring Hill, St Petersburg, Trinity, and Wesley Chapel, where road safety and fall prevention are critical.
- Wearing Seat Belts: Always buckle up, whether you’re the driver or a passenger. Seat belts are your first line of defense in a car accident, preventing your head from striking hard surfaces inside the vehicle.
- Using Helmets: Wear a helmet whenever participating in activities with a risk of head injury. This includes cycling, motorcycling, skateboarding, skiing, snowboarding, and contact sports. A helmet can absorb much of the impact force, protecting your brain.
- Fall-Proofing Homes for Seniors: Falls are a leading cause of TBI, particularly for older adults. Simple modifications like installing grab bars in bathrooms, adding handrails on stairs, removing tripping hazards (rugs, clutter), and ensuring adequate lighting can make a significant difference. Regular vision check-ups and exercise to improve balance also help.
- Avoiding Driving Under the Influence: Never drive after consuming alcohol or drugs that impair your judgment or reaction time. Impaired driving is a major contributor to severe car accidents and resulting TBIs.
- Child Safety: Ensure children wear helmets during activities like biking or scootering. Use appropriate child safety seats in vehicles and install safety gates at the top of stairways and window guards to prevent falls in young children.
The Societal and Economic Impact
The impact of moderate brain injuries extends beyond the individual and their family to society as a whole. The sheer number of incidents and the long-term care required place a substantial burden on healthcare systems and the economy.
As mentioned earlier, the lifetime economic cost of TBI in the United States was estimated to be approximately $76.5 billion (in 2010 dollars). This staggering figure includes direct medical costs—such as emergency services, hospital stays, surgeries, and rehabilitation—as well as indirect costs like lost productivity, unemployment, and the need for long-term care. Fatal TBIs and those requiring hospitalization account for approximately 90% of total TBI medical costs, underscoring the severity and expense associated with more serious brain injuries.
The societal impact also includes the loss of potential contributions from individuals whose lives are altered by TBI, and the strain on social support systems. Understanding this broader picture emphasizes the importance of both prevention efforts and comprehensive support for survivors and their families. You can find more detailed information on the costs of TBIs from the CDC report on TBI costs.
Frequently Asked Questions about Moderate Brain Injury
Can you fully recover from a moderate brain injury?
Recovery varies greatly among individuals. While many people see significant improvement in symptoms over 6-9 months, some may experience lifelong physical, cognitive, or emotional challenges. Rehabilitation plays a crucial role in maximizing recovery. Even with significant improvement, some individuals may experience subtle but lasting changes that impact their daily lives.
What is the difference between a moderate TBI and a concussion?
A concussion is a form of mild TBI. A moderate brain injury is more serious, defined by a longer period of unconsciousness (15 minutes to 6 hours) and/or post-traumatic amnesia (up to 24 hours), and often results in more significant and lasting symptoms. Concussions typically involve a brief or no loss of consciousness and a shorter period of confusion.
How is a moderate brain injury diagnosed?
Diagnosis typically begins in an emergency room and involves a neurological exam to assess function. Doctors use the Glasgow Coma Scale to rate severity and often order imaging tests like a CT scan or MRI to check for bleeding, bruising, or swelling in the brain. The clinical picture, combined with the duration of unconsciousness and post-traumatic amnesia, helps confirm the diagnosis of a moderate brain injury.
Conclusion
A moderate brain injury is a profound event that can significantly alter the course of an individual’s life and impact their family. We’ve explored how it’s defined by specific periods of unconsciousness and memory loss, its common causes ranging from car accidents to falls, and the immediate and long-term physical, cognitive, and emotional effects it can have. The road to recovery is often long and challenging, requiring dedicated rehabilitation and a strong support system.
At Carey Leisure Carney, we understand the immense difficulties faced by those living with a moderate brain injury. We believe that every individual deserves comprehensive support and justice, especially when their injury was caused by another’s negligence. If you or a loved one in Clearwater, Largo, New Port Richey, Spring Hill, St Petersburg, Trinity, or Wesley Chapel, Florida, has suffered a moderate brain injury due to someone else’s carelessness, you may have legal rights to compensation for medical expenses, lost wages, and pain and suffering.
We are here to help you steer the complexities of your situation, ensuring you have direct access to experienced, board-certified attorneys with over 100 years of combined experience. Don’t face this challenging journey alone. Contact our team today for a free consultation to understand your options and secure the future you deserve.
Contact a Traumatic Brain Injury Attorney for a free consultation
